MECHANISM:
Cotrimoxazole is a combination of sulfamethaoxazole + trimethoprim in a ratio of 5:1 .
Sulfamethaoxazole and trimethoprim separately are bacteriostatic drugs but when combined together they become bacteriocidal .
Cotrimoxazole is a bacteriocidal drug.
Bacteriocidal activity is due to sequential blockade .
Sulfamethoxazole inhibit folate synthase and trimethoprim inhibits
folate reductase.
PHARMACOKINETICS:
Cotrimoxazole is a combination of sulfamethaoxazole + trimethoprim in a ratio of 5:1 .
Sulfamethaoxazole and trimethoprim separately are bacteriostatic drugs but when combined together they become bacteriocidal .
Cotrimoxazole is a bacteriocidal drug.
Bacteriocidal activity is due to sequential blockade .
Sulfamethoxazole inhibit folate synthase and trimethoprim inhibits
folate reductase.
PHARMACOKINETICS:
- Taken orally
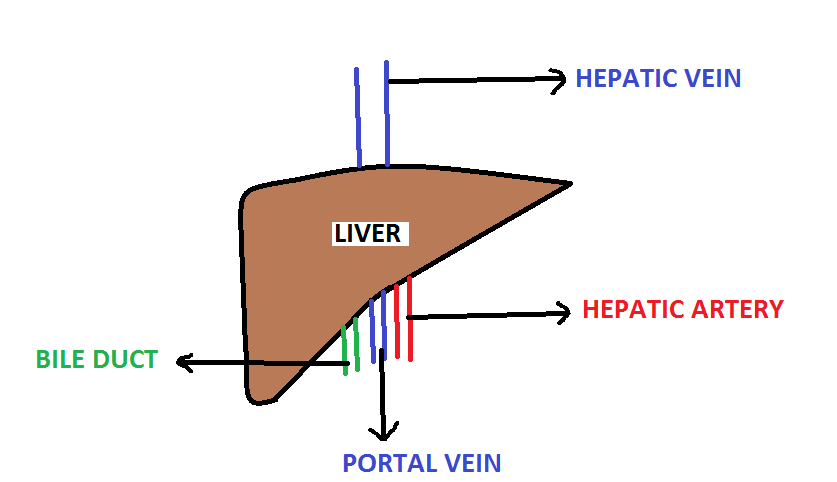
- Metabolized in liver
- Excreted in urine
USE:
- UTI
- RTI
- MRSA
- Drug of choice for Pneumocystitis jirovecii and nocardiosis .
ADVERSE EFFECTS:
It has adverse effects of both sulphonamides and trimethoprim .
SULPHONAMIDE ADVERSE EFFECTS
- Aplastic Anemia
- Bilirubin displacement from plasma protein leading to Kernicterus
- Crystalluria
- Rash
- SLE
- Hemolysis in patients with G-6PD deficiency
TRIMETHOPRIM SIDE EFFECTS
- Megaloblastic Anemia
- Leukopenia
- Pancytopenia
- Hyperkalemia ( due to amiloride like action , amiloride is a Potassium sparing diuretic ).